Have you ever looked in the mirror and wondered why your waistline just won’t shrink, no matter how hard you try? Here’s an estimate: One in three adults has non-alcoholic fatty liver disease, and your liver isn’t just processing that glass of wine. It’s your body’s chemical processing plant, and when it’s clogged with fat, your metabolism drops precipitously. Suddenly, most people don’t realize they’re walking around with fat.
Losing weight can seem like pushing a boulder uphill.
The worst part? People often overlook non-alcoholic fatty liver disease altogether. You could be doing everything “right,” while this silent conspirator is working against you behind the scenes.
So what exactly causes fat to accumulate in your liver, and why does it make losing weight so impossible? The answer may surprise you…
Understanding Non-Alcoholic Fatty Liver Disease (NAFLD)
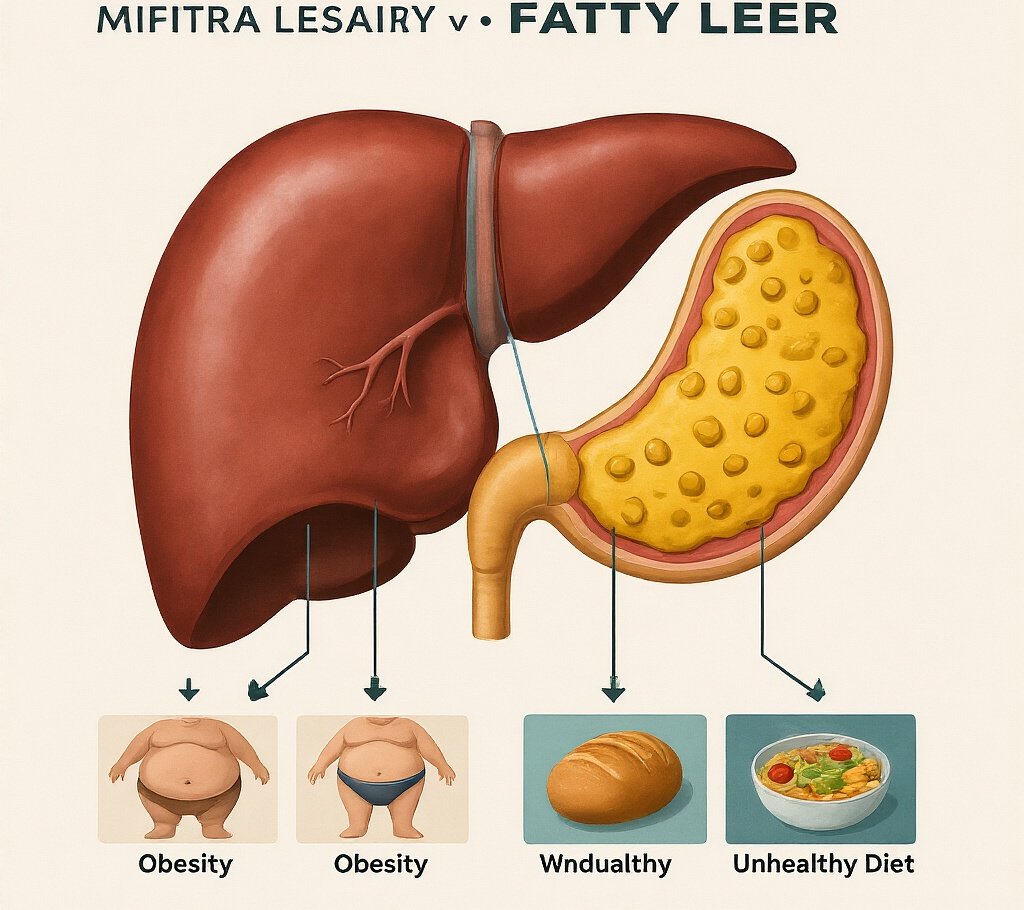
What is NAFLD and why it matters
Your liver is very important – it cleanses your body. But when it stores too much fat (more than 5% fat), you develop non-alcoholic fatty liver disease, or NAFLD.
The truth is, it’s not caused by drinking alcohol. It happens to people who drink little or nothing. Instead, it’s often associated with being overweight, diabetes, high cholesterol or high blood pressure.
Why should you care? Because your liver can’t be lazy. It filters out toxins, processes nutrients, and makes the proteins your body needs to function. When fat gets in the way, these important jobs can’t be done properly. And unlike a sprained ankle, your liver won’t scream when it’s in pain.
Alarming statistics: 1 in 3 adults affected
These statistics are truly shocking. One-third of adults in the US are currently suffering from fatty liver. That’s more than 80 million Americans.
And what’s worse? These statistics are constantly rising, especially among young people. Children are no exception – about 10% of American children now suffer from NAFLD.
The scariest part? Most people suffering from fatty liver do not even know they have this disease.
Signs and Symptoms to watch for
NAFLD is sneaky. Most people feel perfectly fine until things get serious. But here are some hints your liver might be struggling:
- Fatigue that doesn’t go away with rest
- Pain or discomfort in the upper right abdomen
- Unexplained weight loss
- Weakness
- Confusion or trouble concentrating
- Swelling in your abdomen or legs
Don’t panic if you’re tired sometimes – we all are. But persistent symptoms warrant a conversation with your doctor.
Differentiating NAFLD from other liver conditions
NAFLD is just one cause of your liver problems. Let’s find out how it differs from other common liver problems:
| Condition | Main Cause | Key Differences |
| NAFLD | Metabolic factors (obesity, diabetes) | No significant alcohol use |
| Alcoholic Fatty Liver | Excessive alcohol consumption | Drinking history is the giveaway |
| Hepatitis | Viral infections | Usually has different blood markers |
| Autoimmune Hepatitis | Immune system attacking liver | Different pattern of inflammation |
Your doctor can diagnose them with blood tests, imaging, and sometimes a liver biopsy if needed.
The good news? If caught early, NAFLD can often be reversed with lifestyle changes. But you can’t fix a problem you don’t know you have.
Risk Factors and Causes
Obesity and Metabolic Syndrome Connections
You can’t talk about fatty liver without talking about weight. The statistics don’t lie – about 70% of obese people suffer from NAFLD. But it’s not just about what you see on the scale.
When metabolic syndrome starts, this is what happens inside your body. When you have this dangerous trio: high blood pressure, high blood sugar and unhealthy cholesterol levels, your body becomes an inflammation factory.
When your cells stop responding properly to insulin, your liver becomes a repository of excess fat. It’s like your liver becomes a storage center for the fat that your body can’t process anywhere else.
Dietary Triggers that make Fatty Liver Worse
Your liver hates three things: sugar, processed foods, and alcohol. Drinking soda every day? It increases the amount of fructose in your liver which converts straight to fat.
Those convenient ultra-processed foods that contain things you can’t pronounce? They’re an inflammation-causing nightmare for your liver cells.
While a glass of wine might be fine for some, for someone with an already troubled liver, even a little bit of alcohol can add fuel to the fire.
Genetic Predispositions
Some people hit the genetic jackpot — and not in a good way. If your parents or siblings have NAFLD, your risk is greatly increased.
Certain gene variants, such as PNPLA3 and TM6SF2, may make you more susceptible to fat accumulation in your liver, even if you’re not overweight. It’s false, but true.
Lifestyle Factors Contributing to NAFLD
The modern lifestyle is practically designed to create fatty liver:
- Sitting for 8+ hours daily
- High stress levels that trigger stress eating
- Poor sleep that messes with hunger hormones
- Convenience foods replacing home cooking
These aren’t just bad habits – they’re creating the perfect storm for liver damage.
Medical Conditions that Increase Risk
Beyond lifestyle, certain health conditions dramatically increase your NAFLD risk:
- Type 2 diabetes (7 in 10 diabetics have fatty liver)
- PCOS in women
- Hypothyroidism
- Sleep apnea
- Certain medications like corticosteroids and some cancer drugs
Having any of these means you need to be extra vigilant about your liver health.
Diagnosis and Testing
A. When to see a doctor
You’re busy at work when the doctor shows you the results of your routine blood test. He says, “Your liver enzymes are elevated.” This could be the first sign of fatty liver disease.
Don’t ignore these warning signs:
- Persistent fatigue that coffee can’t fix
- Discomfort or pain in the upper right abdomen
- Unexplained weight loss
- Yellowish skin or eyes
- Swelling in your legs or abdomen
The truth is: Many people with fatty liver don’t have any symptoms until the condition becomes severe. So if you have risk factors like diabetes, obesity, high cholesterol, or have ever been a heavy drinker, be sure to get checked out by your doctor.
B. Common Blood Tests and what they Reveal
Your blood tells a story about your liver health:
| Test | What It Measures | What High Levels Might Mean |
| ALT & AST | Liver enzymes released when liver cells are damaged | Active liver inflammation |
| GGT | Another liver enzyme | Potential bile duct issues or alcohol use |
| Albumin | Protein made by liver | Low levels suggest advanced liver problems |
| Bilirubin | Waste product | Possible liver dysfunction |
These tests aren’t perfect. Your numbers could be normal even with fatty liver, or elevated for completely different reasons.
C. Imaging Techniques for Liver Assessment
When blood tests raise eyebrows, your doctor will likely want to take pictures:
Ultrasound is usually first – it’s quick, painless, and can spot fat buildup. Think of it as the liver’s selfie.
More detailed options include:
- Fibroscan: Measures liver stiffness (harder = more scarring)
- CT Scan: Provides 3D views but involves radiation
- MRI: The gold standard for measuring liver fat precisely
D. Liver Biopsy: When it’s Necessary
Nobody gets excited about a liver biopsy. It involves taking a tiny piece of your liver with a needle for examination under a microscope.
The good news? Most people with fatty liver never need one. Doctors typically reserve this for when:
- Your diagnosis remains unclear after other tests
- They need to determine how severe your liver damage is
- They suspect you might have other liver conditions
- You’re being evaluated for experimental treatments
A biopsy is the only way to definitely distinguish NASH (an aggressive form of fatty liver) from simple fatty liver, and determine how much damage has actually occurred.
Why Treating NAFLD is Challenging
A. Limited Pharmaceutical Options
The hard truth? There are no FDA-approved drugs for NAFLD. Not one. Nothing.
When patients are diagnosed, doctors often can’t decide what to prescribe. Most doctors recommend lifestyle changes—better diet, more exercise—but without medications to support these efforts, patients feel alone in their battle with the disease.
Some doctors experiment with off-label drugs like vitamin E or diabetes medications, but results vary from person to person. It’s basically like shooting in the dark and hoping something works.
B. Lack of Specialized Treatment Programs
Try to find a dedicated NAFLD clinic in your area. Good luck.
Most healthcare systems have not created comprehensive programs for these patients. You’ll have to bounce around between your primary care doctor, maybe a gastroenterologist, and possibly a nutritionist—there’s no coordinated care plan linking these visits.
This fragmented approach leaves huge gaps in treatment. Patients feel as if they are putting together puzzle pieces without seeing the whole picture.
C. The Silent Progression of the Disease
Most patients feel nothing as fat slowly accumulates in their livers. No pain. No obvious symptoms. Nothing that screams “Go to the doctor!”
By the time noticeable symptoms appear—fatigue, yellowing skin, a swollen abdomen—a lot of damage has already been done. This silent evolution means people don’t seek treatment until the condition is severe, making intervention even more difficult.
This silent nature also makes motivation for treatment challenging. How do you convince someone to make difficult lifestyle changes for a condition they can’t feel or see?
Effective Strategies for Reversing Fatty Liver
Evidence-Based Dietary Approaches
The truth about treating fatty liver is this: what you eat matters more than anything else. First and foremost, cut back on sugar and refined carbohydrates. These are poison to the liver at this point.
The Mediterranean diet works wonders – several studies show it can reduce liver fat by 20-30% in just a few months. Think olive oil, fish, nuts and lots of colorful vegetables.
Intermittent fasting? It’s not just hype. Going without eating for more than 16 hours causes your liver to stop processing incoming calories and start clearing out stored fat.
What about keto? It works for some people, but its scientific basis isn’t as strong as Mediterranean methods. Plus, it’s difficult to follow long-term.
Exercise Protocol to Reduce Liver Fat
You don’t have to be a marathon runner to heal your liver. Just 150 minutes of moderate exercise a week can reduce liver fat by up to 40%.
HIIT (high-intensity interval training) gives you the most bang for your buck. In several studies, just 20 minutes of exercise three times a week outperformed longer moderate workouts.
Strength training twice a week builds muscle that helps burn fat even while you’re sedentary. Your liver loves it.
Which combination works best? Three days of HIIT cardio, two days of strength training and a daily walk. Your liver will thank you.
Weight Loss Goals That Improve Liver Health
Even modest weight loss can do wonders for your liver. Losing just 5-10% of your body weight can reduce liver fat by up to 40% and dramatically improve symptoms of inflammation.
The best way? Lose weight gradually – about 1-2 pounds per week. Crash diets actually put more stress on your liver.
Waist circumference matters more than the measurement you see on the scale. Men should aim to lose less than 40 inches and women should aim to lose less than 35 inches.
Supplements with Promising Research
Not all liver health supplements are the same:
- Vitamin E (800 IU daily) – solid research shows it reduces liver inflammation
- Milk thistle – used for centuries, but clinical results have been mixed
- Berberine – promising new research shows it improves insulin sensitivity
- Omega-3 (1-2 grams daily) – reduces liver fat and inflammation
Avoid “liver cleanse” products. These are mostly sold without any scientific basis
Tracking your Progress Effectively
Blood tests have a profound effect on emotions. Most important indicators:
- ALT/AST (liver enzymes)
- Triglycerides
- Fasting glucose
- Insulin levels
Get a liver ultrasound fibroscan every 6-12 months to directly measure fat loss.
Focus on the fit of your clothes rather than weighing yourself daily. Daily fluctuations can be annoying and are not really important.
Try tracking your food intake for 2 weeks at first. Most people underestimate their food intake by 30% or even more.
Creating Your NAFLD Recovery Plan
A. Set Realistic Health Goals
Look, being diagnosed with NAFLD can feel overwhelming. But the truth is that small, doable changes lead to big results.
Start with the most important thing: aim to lose 5-10% of your body weight. That’s it. No crazy changes, just a small reduction, which research shows can significantly reduce liver fat.
Break it down into smaller chunks:
- Weeks 1-2: Replace one sugary drink with water every day
- Month 1: Take a 10-minute walk after dinner
- Month 2: Learn three essential liver-healthy recipes to eat on a rotating basis throughout the week
Track your progress with blood tests, not just the scale. ALT and AST levels say more about your liver health than weight alone.
B. Daily Habits that Protect your Liver
Your liver is telling you to rest. These daily habits aren’t complicated, but make a huge difference:
Coffee really helps! 2-3 cups of coffee a day can help reduce liver fat. Just don’t eat the sugary stuff.
Move your body the way you like – take a walk, swim, dance in your kitchen. Aim for 30 minutes of sleep most days, but even 10 minutes is better than no sleep at all.
Sleep matters more than you think. Less sleep promotes inflammation, which your liver doesn’t need. Build a regular bedtime routine.
Food-friendly ways to eat: Eat your biggest meal early in the day and try to go 12+ hours without eating at night to give your liver time to recover.
C. Managing Associated Conditions For Better Outcomes
NAFLD rarely travels alone. It brings friends—and none of them are good news.
If you have these conditions along with NAFLD, treating them also improves your liver health:
- Type 2 Diabetes: Even modest improvements in blood sugar control can reduce liver inflammation.
- Sleep Apnea: Diagnosis and treatment can improve liver enzymes in just a few months.
- Metabolic Syndrome: Tackling high blood pressure and cholesterol reduces pressure on your liver.
Don’t treat these as separate problems. Tell each specialist about your NAFLD and ask specifically how their treatment plan is helping your liver heal.
Remember – improving any one condition has a positive impact on your overall health.
Managing non-alcoholic fatty liver disease requires a comprehensive approach that addresses its root causes. By understanding risk factors, getting a proper diagnosis, and implementing effective strategies like dietary changes and regular exercise, individuals can take control of their liver health. Although treatment can be challenging, the right knowledge and tools can make NAFLD reversible for many patients.
Take the first step today by creating your personalized NAFLD recovery plan. Consult with healthcare providers who specialize in liver health, make lasting lifestyle changes, and monitor your progress regularly. Remember that improving liver health takes time, but with dedication and the right approach, you can lose liver fat and improve your overall health.










Leave a Reply